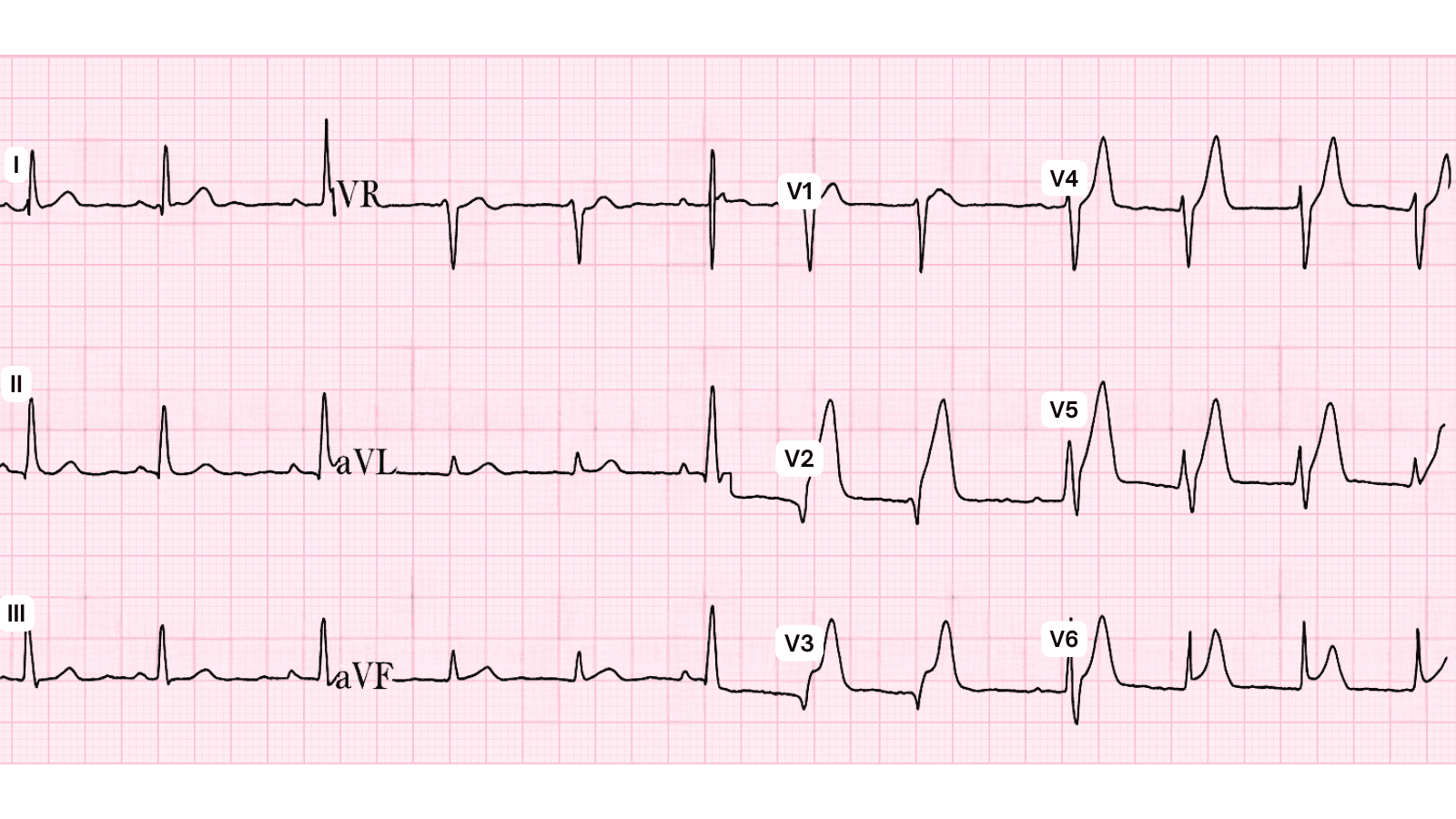
 Anterior MI ECG Example
Figure 1: Anterior MI - Characteristic ECG Pattern
Anterior MI ECG Example
Figure 1: Anterior MI - Characteristic ECG Pattern
🚨 Critical Key Points
- Affected Territory: Anterior MI
- ECG Leads Involved: V1-V4, aVL
- Culprit Artery: Left Anterior Descending (LAD) artery
- Primary Emergency Management: Immediate reperfusion therapy within 90-120 minutes
- Mortality Risk: 15-20% in-hospital mortality if untreated, significantly improved with early reperfusion
Overview and Clinical Significance
Anterior MI is a life-threatening emergency requiring immediate recognition and treatment. Anterior MI typically results from LAD occlusion, affecting the anterior wall of the left ventricle with high risk of complications
Early recognition through systematic ECG analysis and prompt intervention with reperfusion therapy (primary PCI or thrombolytics) significantly reduces mortality and improves long-term outcomes. Every minute of delay increases myocardial damage - "Time is Muscle."
Systematic ECG Recognition
📊 Diagnostic ECG Criteria for Anterior MI
- ST elevation in V1-V4
- Reciprocal ST depression in inferior leads (II, III, aVF)
- New Q waves in anterior leads
- T wave inversion in V1-V4 during evolution
Step-by-Step ECG Analysis
When evaluating any suspected STEMI, follow this systematic approach:
- Rate: Assess heart rate - tachycardia may indicate pump failure, bradycardia common in inferior MI
- Rhythm: Identify any arrhythmias - VT/VF are life-threatening complications requiring immediate defibrillation
- Axis: Check QRS axis for any deviation suggesting prior infarction or conduction abnormalities
- ST Segments: MOST CRITICAL - identify ST elevation ≥1mm in limb leads or ≥2mm in precordial leads in ≥2 contiguous leads
- Reciprocal Changes: Look for ST depression in leads opposite to infarct territory (increases diagnostic certainty)
- Q Waves: Pathologic Q waves indicate transmural infarction (>0.04s duration, >25% of R wave amplitude)
- T Waves: Hyperacute T waves (tall, peaked) in early STEMI; inverted T waves in evolved/subacute phase
- Compare to Prior ECGs: Essential to differentiate acute vs chronic changes, aneurysm, or LBBB
ECG Pattern Variations
The following images demonstrate different presentations and evolutionary stages of Anterior MI:
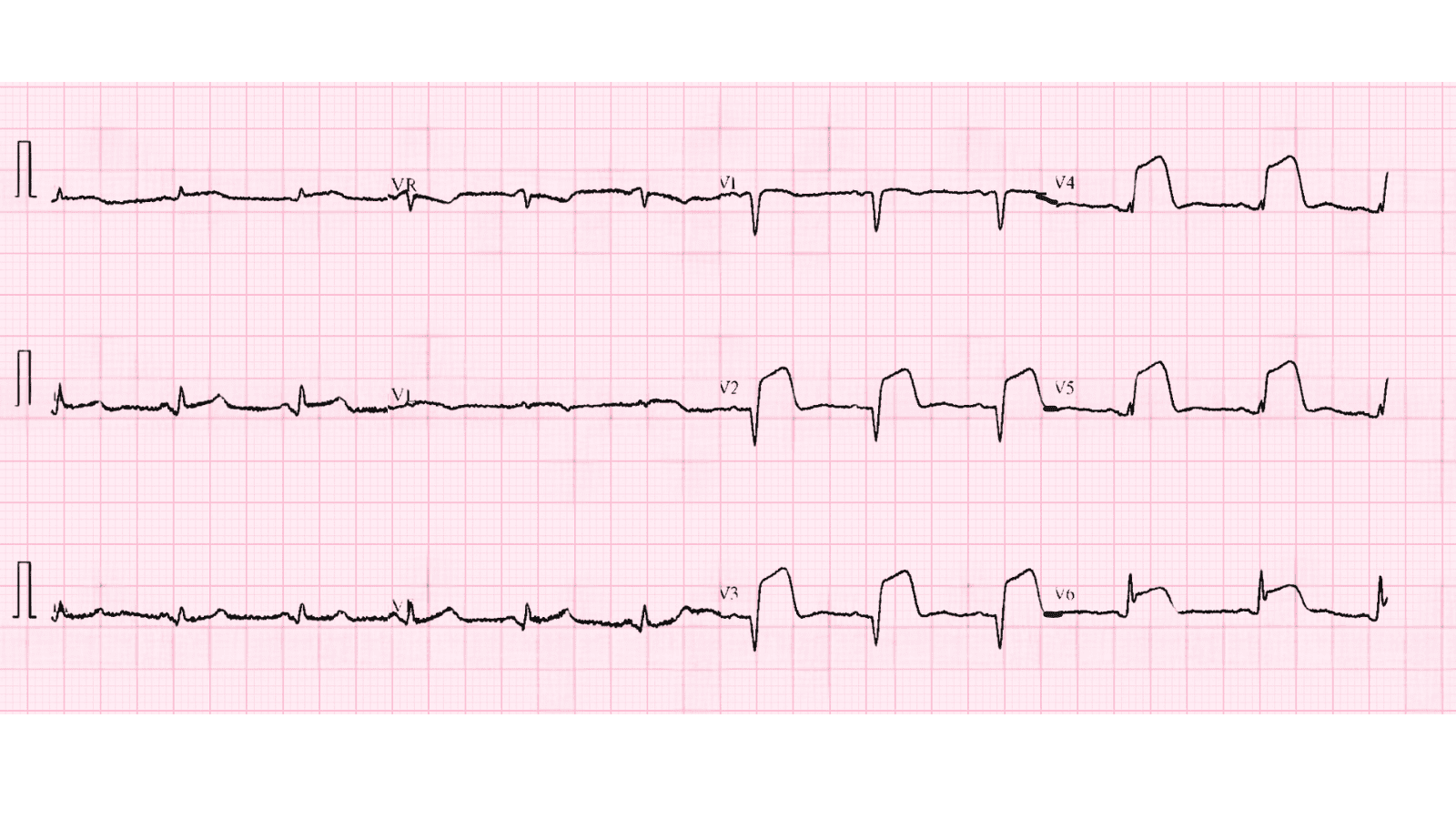 Anterior MI Variation 2
Figure 2: Alternative ECG Pattern
Anterior MI Variation 2
Figure 2: Alternative ECG Pattern
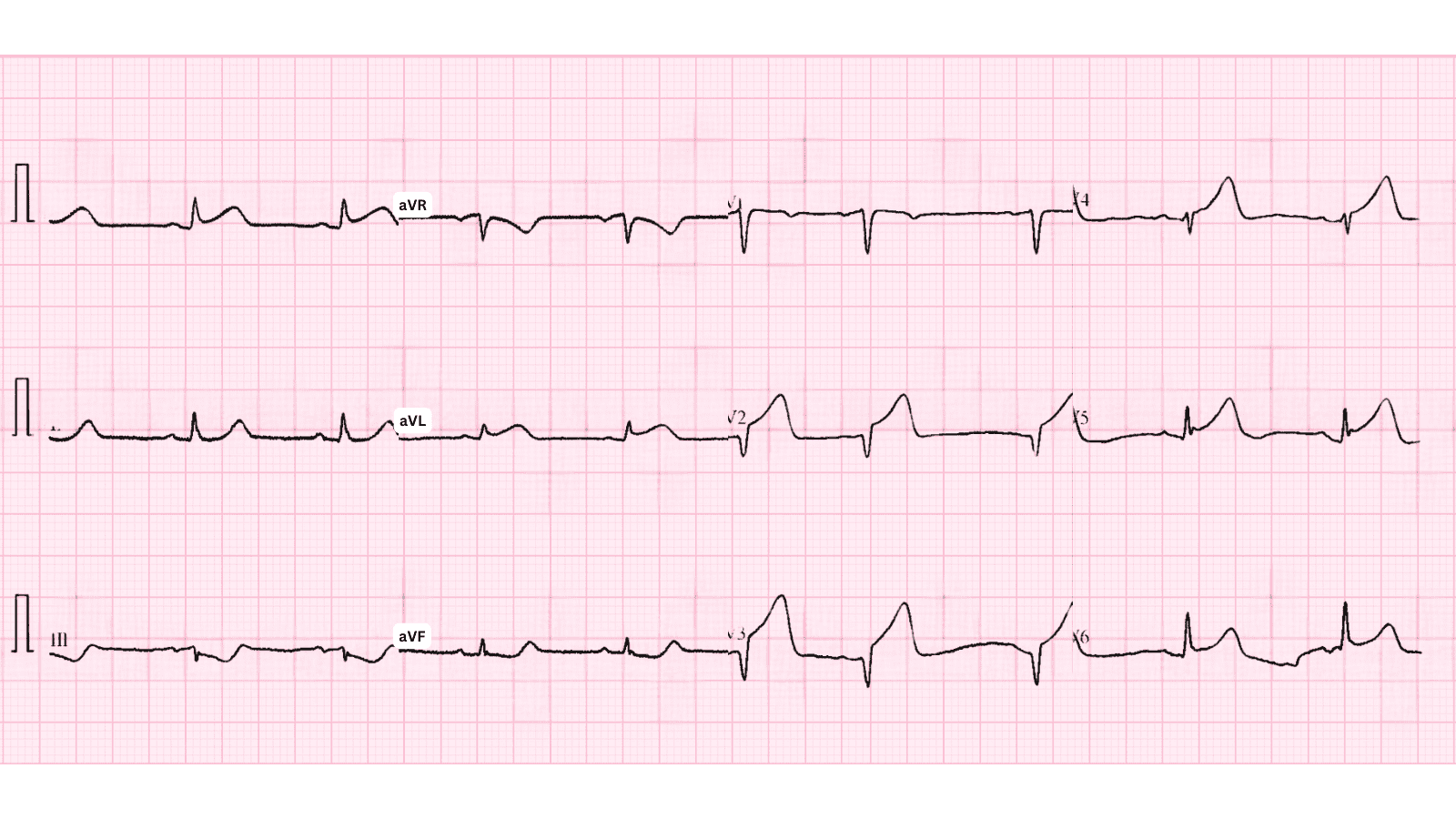 Anterior MI Variation 3
Figure 3: Alternative ECG Pattern
Anterior MI Variation 3
Figure 3: Alternative ECG Pattern
Pathophysiology and Mechanisms
Anterior MI occurs when there is complete occlusion of the Left Anterior Descending (LAD) artery, leading to transmural myocardial ischemia and necrosis. The ischemic cascade progresses rapidly:
- 0-20 minutes: Reversible ischemia, metabolic changes, diastolic dysfunction
- 20-40 minutes: Irreversible cell injury begins, systolic dysfunction develops
- 2-4 hours: Transmural necrosis, ST elevation on ECG, troponin release
- 6-12 hours: Inflammatory response, increased risk of arrhythmias and mechanical complications
- Days to weeks: Healing, scar formation, ventricular remodeling
💡 Clinical Pearl
In STEMI, the "golden hour" is critical - mortality increases 1% for every 30-minute delay in reperfusion. Door-to-balloon time goal is <90 minutes for primary PCI, door-to-needle time <30 minutes for thrombolytics.
Evidence-Based Emergency Management
Immediate Life-Saving Interventions
🚨 STEMI Emergency Protocol - First 10 Minutes
- Activate STEMI team immediately - do not delay for troponin results
- Obtain 12-lead ECG within 10 minutes of arrival (prehospital ECG ideal)
- Administer aspirin 162-325mg chewed (unless contraindicated)
- Provide supplemental oxygen if SpO₂ <90% (avoid hyperoxia)
- Establish large-bore IV access (×2) and obtain stat labs (troponin, CBC, BMP, coags, lipid panel)
- Administer sublingual nitroglycerin for chest pain (avoid in RV infarct, inferior MI with hypotension)
- Morphine 2-4mg IV for refractory chest pain (use cautiously - may mask symptoms)
- Decide reperfusion strategy: Primary PCI (preferred) vs thrombolytics
Reperfusion Therapy
Primary Strategy: Immediate reperfusion therapy (primary PCI preferred, thrombolytics if PCI unavailable within 120 min), dual antiplatelet therapy, anticoagulation, beta-blockers, ACE inhibitors
Primary PCI (Preferred Method):
- Goal: Door-to-balloon time <90 minutes (60 minutes for cardiogenic shock)
- Superior to thrombolytics - lower mortality, reduced reinfarction and stroke rates
- Radial access preferred over femoral (reduced bleeding complications)
- Routine thrombus aspiration NOT recommended
- Drug-eluting stents are standard of care
Fibrinolytic Therapy (if PCI unavailable within 120 minutes):
- Goal: Door-to-needle time <30 minutes
- Best if given within 3 hours of symptom onset (diminishing benefit after 12 hours)
- Agents: Tenecteplase (TNK), Alteplase (tPA), Reteplase (preferred: TNK for ease of use)
- Transfer to PCI-capable center after lysis for angiography (pharmacoinvasive strategy)
Adjunctive Pharmacotherapy
Medication Dosing Indication Aspirin 162-325mg chewed, then 81mg daily All STEMI patients (Class I) P2Y12 Inhibitor Ticagrelor 180mg load OR Prasugrel 60mg OR Clopidogrel 600mg Dual antiplatelet therapy (Class I) Anticoagulation Heparin or Bivalirudin during PCI Prevent thrombosis (Class I) Beta-blocker Metoprolol 25-50mg PO (avoid if shock/HF) Reduce arrhythmias, reduce mortality (Class I) ACE Inhibitor Lisinopril 2.5-5mg PO within 24h Prevent remodeling, reduce mortality (Class I) Statin Atorvastatin 80mg PO High-intensity statin (Class I)
Complications and Risk Stratification
Common Complications of Anterior MI:
High risk of pump failure, cardiogenic shock, ventricular aneurysm formation
Additional life-threatening complications requiring vigilance:
- Cardiogenic shock: 5-10% of STEMI patients, 50% mortality despite treatment - requires intra-aortic balloon pump or mechanical circulatory support
- Ventricular free wall rupture: Usually 3-5 days post-MI, sudden hemodynamic collapse, requires emergency pericardiocentesis and surgery
- Ventricular septal defect: New harsh holosystolic murmur, biventricular failure - emergency surgical repair
- Acute mitral regurgitation: Papillary muscle rupture or dysfunction - pulmonary edema, new murmur - may require emergent surgery
- Malignant arrhythmias: VT/VF in first 48 hours (common), complete heart block (especially inferior MI), atrial fibrillation with rapid rate
📅 Post-STEMI Management and Follow-Up
- Hospital stay: CCU monitoring for 24-48 hours minimum, telemetry until stable
- Risk stratification: Echocardiogram to assess EF, wall motion abnormalities, complications
- Cardiac rehabilitation: Enrollment prior to discharge - improves outcomes and quality of life
- Cardiology follow-up: Within 7-14 days post-discharge for medication optimization
- Lifestyle modifications: Smoking cessation (most important!), diet, exercise, weight loss, stress management
- Secondary prevention: Lifelong DAPT (minimum 12 months), statin, beta-blocker, ACE-I/ARB, aspirin
Common Pitfalls and How to Avoid Them
⚠️ Critical Mistakes That Cost Lives
- Waiting for troponin results before activating cath lab - ECG is diagnostic, troponins lag behind injury by hours
- Dismissing atypical presentations - women, elderly, diabetics often present without chest pain (dyspnea, nausea, fatigue)
- Missing LBBB-associated STEMI - use Sgarbossa criteria (concordant ST elevation ≥1mm, concordant ST depression ≥1mm in V1-V3, or discordant ST elevation ≥5mm)
- Giving beta-blockers in RV infarction - can precipitate profound hypotension and cardiovascular collapse
- Under-treating pain with inadequate analgesia - pain increases sympathetic tone, worsening ischemia
- Delaying reperfusion for "stable" patients - even asymptomatic STEMI requires urgent intervention
- Failing to recognize cardiogenic shock early - signs: SBP <90mmHg, cool extremities, altered mentation, oliguria
Patient Education and Discharge Instructions
Comprehensive patient counseling is essential for secondary prevention and long-term success:
- Warning signs of recurrent MI: Chest pain/pressure, shortness of breath, diaphoresis, nausea - call 911 immediately, do NOT drive yourself
- Medication adherence: Emphasize critical importance of DAPT - stopping early dramatically increases stent thrombosis risk (often fatal)
- Activity progression: Gradual return to normal activities as tolerated, cardiac rehab participation strongly encouraged
- Sexual activity: Generally safe to resume 1-2 weeks post-MI if able to climb 2 flights of stairs without symptoms
- Driving restrictions: Typically 1 week for stable patients, longer if complications or ICD placement
- Return to work: Usually 2-6 weeks depending on occupation and cardiac function
- Psychological support: Post-MI depression is common (30%), screening and treatment improve outcomes
Evidence-Based Guidelines
Current STEMI management is supported by high-quality evidence from landmark trials and consensus guidelines:
- ACC/AHA STEMI Guidelines (2023) - Comprehensive evidence-based recommendations
- European Society of Cardiology (ESC) STEMI Guidelines - International perspective and evidence
- DANAMI-2 Trial - Demonstrated superiority of primary PCI over fibrinolysis
- HORIZONS-AMI Trial - Bivalirudin vs heparin in STEMI
- TRITON-TIMI 38 - Prasugrel vs clopidogrel in ACS
- PLATO Trial - Ticagrelor vs clopidogrel showing mortality benefit
📚 Level of Evidence
Primary PCI for STEMI is supported by Level A evidence (multiple high-quality randomized controlled trials and meta-analyses). Door-to-balloon time <90 minutes is a Class I recommendation (should be performed).
Summary and Clinical Bottom Line
📋 Clinical Bottom Line
Anterior MI is a life-threatening emergency characterized by ST elevation in V1-V4, aVL indicating acute occlusion of the Left Anterior Descending (LAD) artery. Immediate Action: Activate STEMI team, give aspirin and P2Y12 inhibitor, proceed to emergency coronary angiography with primary PCI (goal door-to-balloon <90 minutes). Key Complication: High risk of pump failure, cardiogenic shock, ventricular aneurysm formation Remember: Time is muscle - every minute counts. Early recognition and rapid reperfusion save lives and preserve cardiac function.
About the Author
Dr. Raj K
Emergency Medicine Physician Dr. Raj K is a board-certified Emergency Medicine physician with extensive experience in acute cardiac emergencies, STEMI management, and advanced ECG interpretation. He has managed hundreds of STEMI cases and is passionate about teaching evidence-based emergency cardiology through E-PulsePoints. His expertise includes primary PCI coordination, mechanical circulatory support, and complex coronary interventions.