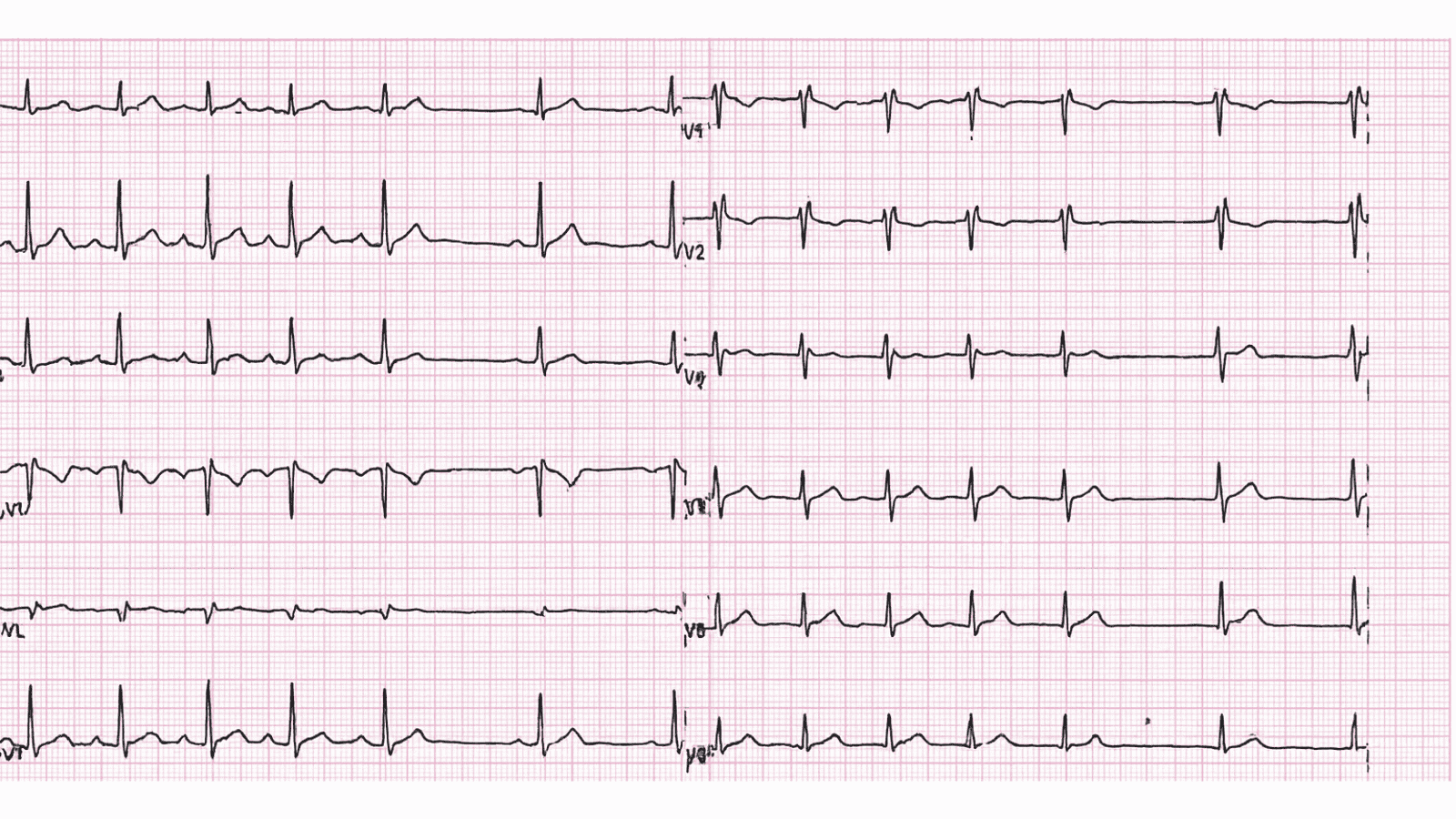
 Incomplete Right Bundle Branch Block ECG Example
Figure 1: Incomplete Right Bundle Branch Block - Characteristic ECG Pattern
Incomplete Right Bundle Branch Block ECG Example
Figure 1: Incomplete Right Bundle Branch Block - Characteristic ECG Pattern
🔑 Key Points at a Glance
- Heart Rate: Normal sinus rhythm (60-100 bpm)
- Primary Significance: Often benign, may indicate RV strain, common in athletes and normal individuals
- Key Management: Usually no treatment required, evaluate for underlying structural heart disease if symptomatic, consider RV pathology
- Clinical Category: Education
Overview and Clinical Significance
Incomplete Right Bundle Branch Block represents an important cardiac rhythm pattern that clinicians must accurately identify. Often benign, may indicate RV strain, common in athletes and normal individuals
Understanding this ECG finding is essential for emergency physicians, cardiologists, intensivists, and all healthcare providers involved in acute cardiac care. Early recognition and appropriate management can significantly impact patient outcomes and prevent life-threatening complications.
ECG Characteristics and Recognition
📊 Diagnostic ECG Criteria
- RSR' pattern in V1-V2
- QRS duration 100-120ms (incomplete)
- Terminal R wave in V1
- Slurred S wave in lateral leads
Systematic ECG Analysis Approach
When analyzing any ECG, including suspected Incomplete Right Bundle Branch Block, follow this systematic approach:
- Rate: Calculate ventricular rate using the 300-150-100-75-60-50 rule or count QRS complexes in 6 seconds × 10
- Rhythm: Assess regularity by measuring R-R intervals across the entire strip
- P Waves: Identify presence, morphology, and relationship to QRS complexes
- PR Interval: Measure from start of P wave to start of QRS (normal: 0.12-0.20 seconds or 3-5 small squares)
- QRS Complex: Assess duration (normal: Most patients with this ECG finding are asymptomatic - focus on proper documentation and patient education
Evidence-Based Management
Acute Management Strategy
Primary Treatment Approach: Usually no treatment required, evaluate for underlying structural heart disease if symptomatic, consider RV pathology
Stepwise Treatment Algorithm
Step 1: Initial Stabilization
- Ensure hemodynamic stability - check blood pressure, perfusion, mental status
- Obtain IV access and send labs (troponin, BMP, CBC, coags, BNP if heart failure suspected)
- Continuous telemetry monitoring in appropriate care setting
- Serial ECGs to assess for dynamic changes
Step 2: Definitive Management
Usually no treatment required, evaluate for underlying structural heart disease if symptomatic, consider RV pathology
Pharmacologic Interventions
Most cases require no specific pharmacologic intervention - focus on treating underlying causes and monitoring for progression.
Differential Diagnosis and ECG Mimics
🔍 Consider These Alternative Diagnoses
- Similar ECG patterns to distinguish from: Careful analysis of specific ECG criteria, clinical context, and patient presentation is essential for accurate diagnosis
- Use systematic approach: Compare rate, rhythm, P wave morphology, PR interval, QRS width, and ST-T changes
- When in doubt: Obtain cardiology consultation, compare to old ECGs, correlate with clinical presentation
Complications and Risk Stratification
Potential complications and adverse outcomes associated with Incomplete Right Bundle Branch Block:
- Immediate risks: Generally minimal immediate risk in most patients
- Short-term complications: Syncope, pre-syncope, fatigue, reduced exercise tolerance
- Long-term sequelae: Tachycardia-induced cardiomyopathy if persistent, quality of life impact
Long-Term Management and Follow-Up
Routine follow-up is generally not required unless symptoms develop or underlying cardiac disease is suspected.
📅 Follow-Up Recommendations
- Primary care follow-up as needed for routine health maintenance
- Repeat ECG only if clinically indicated
- Lifestyle modifications: regular exercise, stress reduction, adequate sleep, avoid triggers (caffeine, alcohol, stimulants)
- Patient education on warning symptoms requiring immediate medical attention
Common Pitfalls and How to Avoid Them
⚠️ Critical Mistakes to Avoid
- Misdiagnosis risk: Always compare to prior ECGs when available - new findings are more significant than chronic changes
- Treatment errors: Avoid treating the ECG in isolation - clinical context and hemodynamic status determine urgency
- Delayed recognition: Unstable patients require immediate intervention, not prolonged workup
- Medication errors: Check medication interactions and contraindications before administration
- Disposition errors: Ensure appropriate level of care and monitoring based on risk stratification
Patient Education and Shared Decision-Making
When counseling patients diagnosed with Incomplete Right Bundle Branch Block, address these important topics:
- Diagnosis explanation: Use simple language avoiding medical jargon - "Your heart's electrical system shows..." rather than complex terminology
- Prognosis discussion: Reassure about benign nature, excellent long-term prognosis, and low risk of complications
- Warning signs: Teach patients to recognize symptoms requiring immediate emergency care (chest pain, severe shortness of breath, syncope, palpitations with dizziness)
- Medication adherence: Typically no long-term medications required
- Lifestyle modifications: Limit caffeine and alcohol, maintain healthy weight through diet and exercise, stress management techniques, adequate sleep hygiene
- Activity guidance: No activity restrictions - encourage normal physical activity and exercise
- Family screening: Discuss cardiovascular risk factors with family members
Evidence-Based Guidelines and Key Trials
Current management of Incomplete Right Bundle Branch Block is based on high-quality evidence from landmark clinical trials and consensus guidelines from major professional societies:
- American Heart Association (AHA) / American College of Cardiology (ACC) - Comprehensive guidelines for cardiac rhythm management
- European Society of Cardiology (ESC) - Evidence-based recommendations for arrhythmia management
- Advanced Cardiac Life Support (ACLS) - Standardized protocols for emergency cardiac care
- Heart Rhythm Society (HRS) - Expert consensus statements on electrophysiology and device therapy
📚 Level of Evidence
Recommendations for management of Incomplete Right Bundle Branch Block are primarily supported by Level C evidence (expert consensus, case series, and standard of care practices).
Summary and Clinical Bottom Line
📋 Clinical Bottom Line
Incomplete Right Bundle Branch Block is characterized by rsr' pattern in v1-v2 on ECG. Often benign, may indicate RV strain, common in athletes and normal individuals Primary management: Usually no treatment required, evaluate for underlying structural heart disease if symptomatic, consider RV pathology Key takeaway: Recognition, documentation, and patient reassurance are the primary interventions - excellent prognosis
About the Author
Dr. Raj K
Emergency Medicine Physician Dr. Raj K is a board-certified Emergency Medicine physician with extensive experience in acute cardiac emergencies, advanced ECG interpretation, and critical care. He is passionate about medical education and bringing evidence-based emergency medicine knowledge to healthcare providers worldwide through E-PulsePoints. His clinical expertise includes STEMI management, complex arrhythmia recognition, and emergency cardiac procedures.