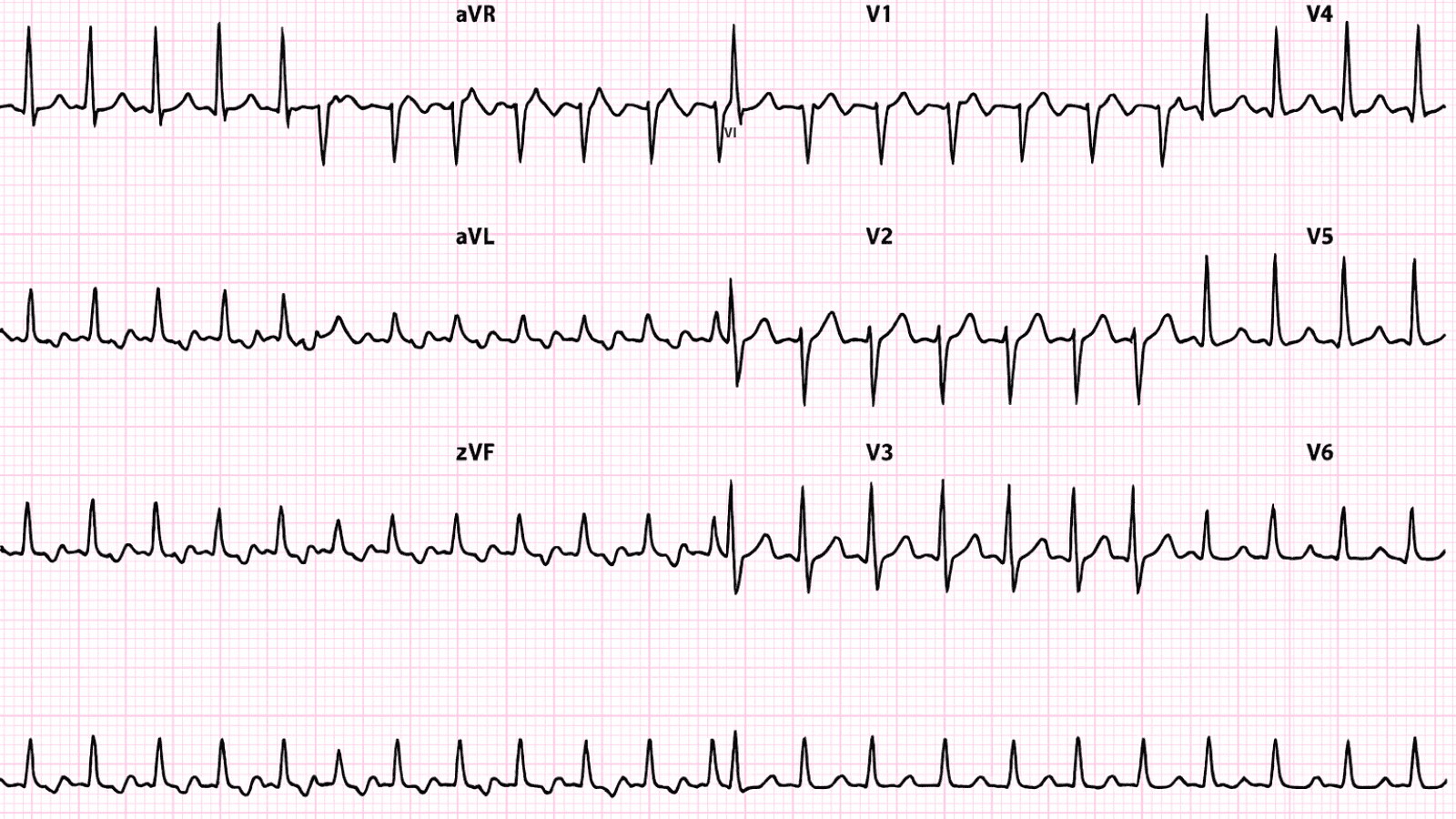
 Wolff-Parkinson-White Syndrome (WPW) ECG Example
Figure 1: Wolff-Parkinson-White Syndrome (WPW) - Characteristic ECG Pattern
Wolff-Parkinson-White Syndrome (WPW) ECG Example
Figure 1: Wolff-Parkinson-White Syndrome (WPW) - Characteristic ECG Pattern
🔑 Key Points at a Glance
- Heart Rate: Variable, can have SVT 150-250 bpm
- Primary Significance: Accessory pathway (Bundle of Kent), risk of rapid pre-excited AFib leading to VFib and sudden death
- Key Management: Avoid AV nodal blockers in pre-excited AFib (use procainamide), catheter ablation curative (>95% success), EP study if symptomatic
- Clinical Category: Clinical
Overview and Clinical Significance
Wolff-Parkinson-White Syndrome (WPW) represents a critical cardiac rhythm pattern that requires immediate recognition and intervention. Accessory pathway (Bundle of Kent), risk of rapid pre-excited AFib leading to VFib and sudden death
Understanding this ECG finding is essential for emergency physicians, cardiologists, intensivists, and all healthcare providers involved in acute cardiac care. Early recognition and appropriate management can significantly impact patient outcomes and prevent life-threatening complications.
ECG Characteristics and Recognition
📊 Diagnostic ECG Criteria
- **Short PR interval Always assess hemodynamic stability FIRST - unstable patients require immediate intervention regardless of the specific ECG diagnosis
Evidence-Based Management
Acute Management Strategy
Primary Treatment Approach: Avoid AV nodal blockers in pre-excited AFib (use procainamide), catheter ablation curative (>95% success), EP study if symptomatic
🚨 Emergency Protocol - Time-Critical Actions
- Immediate ABC assessment (Airway, Breathing, Circulation)
- Attach continuous cardiac monitoring and obtain 12-lead ECG
- Establish large-bore IV access (×2) and check bedside glucose
- Administer supplemental oxygen if SpO₂ 95% success), EP study if symptomatic
Pharmacologic Interventions
Most cases require no specific pharmacologic intervention - focus on treating underlying causes and monitoring for progression.
Differential Diagnosis and ECG Mimics
🔍 Consider These Alternative Diagnoses
- Similar ECG patterns to distinguish from: Careful analysis of specific ECG criteria, clinical context, and patient presentation is essential for accurate diagnosis
- Use systematic approach: Compare rate, rhythm, P wave morphology, PR interval, QRS width, and ST-T changes
- When in doubt: Obtain cardiology consultation, compare to old ECGs, correlate with clinical presentation
Complications and Risk Stratification
Potential complications and adverse outcomes associated with Wolff-Parkinson-White Syndrome (WPW):
- Immediate risks: Cardiac arrest, hemodynamic collapse, sudden cardiac death
- Short-term complications: Syncope, pre-syncope, fatigue, reduced exercise tolerance
- Long-term sequelae: Chronic heart failure, ventricular remodeling, need for ICD/pacemaker
Long-Term Management and Follow-Up
Patients require close cardiology/electrophysiology follow-up with consideration for ICD placement, cardiac rehabilitation, and aggressive risk factor modification.
📅 Follow-Up Recommendations
- Cardiology/EP consultation within 1-7 days post-discharge
- Repeat ECG, echocardiogram, stress test or cardiac MRI as indicated
- Lifestyle modifications: regular exercise, stress reduction, adequate sleep, avoid triggers (caffeine, alcohol, stimulants)
- Implantable device management (ICD/pacemaker interrogation every 3-6 months)
Common Pitfalls and How to Avoid Them
⚠️ Critical Mistakes to Avoid
- Misdiagnosis risk: Always compare to prior ECGs when available - new findings are more significant than chronic changes
- Treatment errors: Avoid treating the ECG in isolation - clinical context and hemodynamic status determine urgency
- Delayed recognition: Unstable patients require immediate intervention, not prolonged workup
- Medication errors: Avoid AV nodal blockers in pre-excited atrial fibrillation (can precipitate VFib)
- Disposition errors: Never discharge home - requires admission to monitored bed
Patient Education and Shared Decision-Making
When counseling patients diagnosed with Wolff-Parkinson-White Syndrome (WPW), address these important topics:
- Diagnosis explanation: Use simple language avoiding medical jargon - "Your heart's electrical system shows..." rather than complex terminology
- Prognosis discussion: Emphasize seriousness but reassure about effective treatment options and survival with appropriate therapy
- Warning signs: Teach patients to recognize symptoms requiring immediate emergency care (chest pain, severe shortness of breath, syncope, palpitations with dizziness)
- Medication adherence: Critical importance of consistent medication compliance - missing doses can have serious consequences
- Lifestyle modifications: Limit caffeine and alcohol, maintain healthy weight through diet and exercise, stress management techniques, adequate sleep hygiene
- Activity guidance: Discuss driving restrictions (varies by state - typically 3-6 months post-event), return to work timeline, sexual activity precautions
- Family screening: Consider genetic counseling and family member screening for hereditary conditions
Evidence-Based Guidelines and Key Trials
Current management of Wolff-Parkinson-White Syndrome (WPW) is based on high-quality evidence from landmark clinical trials and consensus guidelines from major professional societies:
- American Heart Association (AHA) / American College of Cardiology (ACC) - Comprehensive guidelines for cardiac rhythm management
- European Society of Cardiology (ESC) - Evidence-based recommendations for arrhythmia management
- Advanced Cardiac Life Support (ACLS) - Standardized protocols for emergency cardiac care
- Heart Rhythm Society (HRS) - Expert consensus statements on electrophysiology and device therapy
📚 Level of Evidence
Recommendations for management of Wolff-Parkinson-White Syndrome (WPW) are primarily supported by Level A evidence (multiple high-quality randomized controlled trials and meta-analyses).
Summary and Clinical Bottom Line
📋 Clinical Bottom Line
Wolff-Parkinson-White Syndrome (WPW) is characterized by short pr interval 95% success), EP study if symptomatic Key takeaway: This is a life-threatening emergency requiring immediate recognition and treatment - time-critical intervention saves lives
About the Author
Dr. Raj K
Emergency Medicine Physician Dr. Raj K is a board-certified Emergency Medicine physician with extensive experience in acute cardiac emergencies, advanced ECG interpretation, and critical care. He is passionate about medical education and bringing evidence-based emergency medicine knowledge to healthcare providers worldwide through E-PulsePoints. His clinical expertise includes STEMI management, complex arrhythmia recognition, and emergency cardiac procedures.